HAE is a rare autosomal dominant disease affecting approximately 1 in 50,000 individuals worldwide.1,3
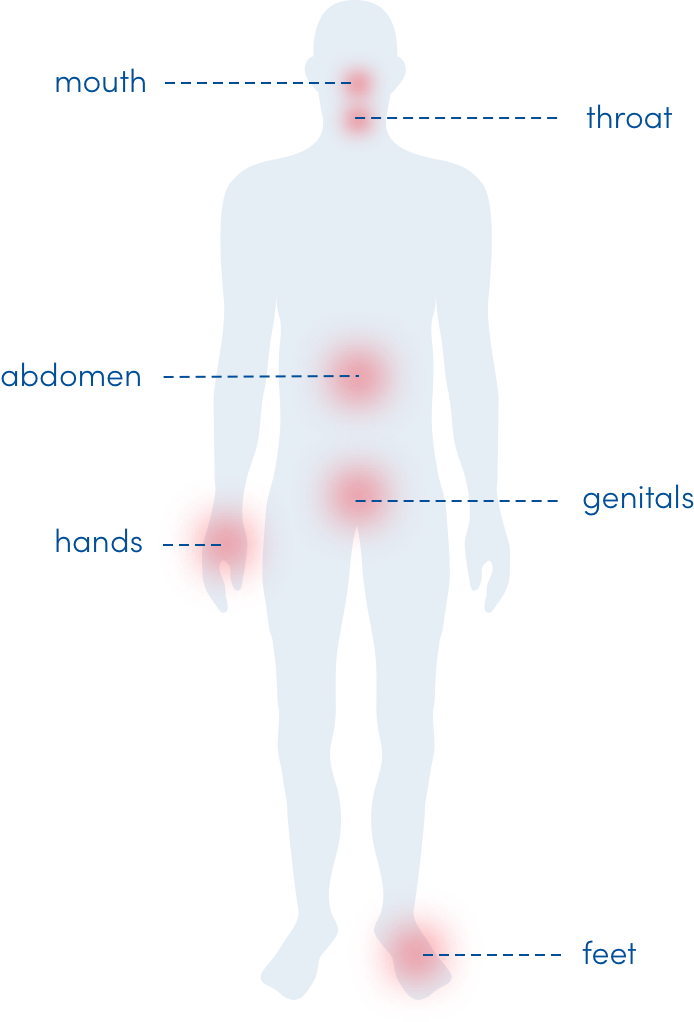
It causes spontaneous attacks of swelling in various parts of the body.3,4
Attacks of swelling are unpredictable in frequency and severity, and they can be life threatening when they occur in the throat.4,5
The disease burden of HAE may extend beyond attacks into everyday life. Due to its unpredictable nature, HAE can cause substantial emotional, psychosocial, and quality-of-life impairments for some patients and their caregivers.2,6
Share this fact sheet with others in your practice to help familiarise them with the signs and symptoms of HAE
Common HAE attack locations3,4
what can cause hereditary angioedema attacks?
There are several different forms of HAE that are currently recognised and genetically identifiable. The two most common are:
C1-INH deficiency (Type 1 HAE, HAE-1):
characterised by low antigenic and functional C1-INH levels
C1-INH dysfunction (Type 2 HAE, HAE-2):
characterised by normal or elevated antigenic but low functional 7 C1-INH levels
Within the kallikrein-kinin system, C1-INH inhibits the production of bradykinin by interfering with plasma kallikrein activity. Dysregulation of plasma kallikrein activity within the kallikrein-kinin system leads to the cleavage of high-molecular-weight kininogen and excess bradykinin production, which can lead to attacks.8,9
Types of HAE4
Other forms of HAE that do not involve mutations of C1-INH include, but are not limited to:
- F12 gene mutation (HAE-FXII)7
- Angiopoietin-1 gene mutation (HAE-ANGPTI)7
- Plasminogen gene mutation (HAE-PLG)7
triggers and prodromal symptoms of hereditary angioedema
While many occur with no identifiable trigger, some HAE attacks may be associated with10:
- Emotional distress
- Physical trauma
- Changes in hormone levels
- Infection
- Medication
- Exposure to cold
- Non-traumatic tissue compression
- Prolonged sitting or standing
- Certain foods
Prodromes can be predictive of an attack in some cases and are often described as11-13:
- Fatigue or malaise
- Restlessness
- Nausea
- Joint pain
- Cramps
- Anxiety or mood changes
The patient may also experience a prickling sensation, tightness in the skin, or nonpruritic rash called erythema marginatum.12-14
Attack history is not a predictor of future attack frequency, severity, or location.5